
It is believed that diabetes develops in those who consume a lot of sweets. In fact, it is a much more complex pathology that only partially depends on nutrition and can develop in any person.
Diabetes mellitus: definition of the disease
Diabetes mellitus (DM) is a group of diseases associated with metabolic disorders. People with diabetes cannot properly digest carbohydrates. As a result, their glucose (blood sugar) concentration rises significantly.
Glucose is a type of sugar that serves as the body's main source of energy.
Excess glucose has a toxic effect and destroys the walls of blood vessels, nerve fibers and internal organs.
Diabetes mellitus develops for various reasons. Some types of disease are genetic in origin, while others are related to lifestyle or environmental factors.
The name of the disease was given by the ancient Greeks. Translated from Greek, διαβαίνω means "to pass", which refers to the main symptom of diabetes mellitus, polyuria or frequent urination. Therefore, a person is constantly losing fluid and seeks to restore it by drinking as much water as possible.
However, this is not always the case. Some forms of diabetes can develop without symptoms for a long time or appear so mild that a person does not even notice that something has gone wrong. And even with the typical course of the disease, many years often pass before the excess glucose in the blood leads to the development of symptoms of the disease. In addition, all this time the person is in a state of hyperglycemia, and at the time of diagnosis there are already severe irreversible disorders of the kidneys, blood vessels, brain, peripheral nerves and retina.
The disease causes significant damage to the body. Without treatment, excess glucose can lead to deterioration of kidney, heart and nerve cell function. But such complications can be prevented. Modern doctors have enough effective drugs and techniques to treat diabetes.
Distribution
In 2019, diabetes was the direct cause of 1. 5 million deaths worldwide. In addition, in almost half of the cases, the disease is fatal in people under the age of 70. The other half of the patients died from complications of the disease: kidney failure, heart and vascular damage.

Besides humans, animals also suffer from diabetes. For example dogs and cats.
From 2000 to 2019, diabetes mortality increased by 3% in developed countries and by 13% in lower-middle-income countries. At the same time, the probability of death from complications of the disease in people aged 30 to 70 years has decreased by 22% worldwide. It is believed that this is due to the improved diagnosis of diabetes and the effective methods of early prevention of its complications.
Classification of diabetes
We use the classification of diabetes mellitus approved by the World Health Organization in 1999.
Diabetes mellitus type I
In this type of disease, a person's pancreas produces little of the hormone insulin, which is needed to transport glucose into cells. As a result, the glucose entering the blood cannot be completely absorbed by the cells, remains in the vessels, is transported to the tissues and gradually destroys them.
Depending on the cause of pancreatic dysfunction, type I diabetes is divided into two subtypes: immune-mediated and idiopathic.
Immune-mediated diabetes mellitusresult from autoimmune destruction of pancreatic cells, causing the immune system to mistakenly attack its own healthy tissue. Diabetes usually begins in childhood or adolescence, but can develop in people of all ages.
Immune-mediated diabetes is often associated with other autoimmune diseases, such as Graves' disease, Hashimoto's thyroiditis, Addison's disease, vitiligo, or pernicious anemia.

Type 1 diabetes most often develops in children and adolescents, although it can occur at any age.
Idiopathic diabetes mellitus.A rare variant of the disease. Such patients do not have laboratory signs of autoimmune damage, but symptoms of absolute insulin deficiency are observed.
Diabetes mellitus type II
In this case, the pancreas produces enough insulin, but the cells are insensitive or resistant to it, so they cannot absorb the glucose and it accumulates in the blood.
Depending on the underlying cause, type II diabetes mellitus is divided into type II diabetes mellitus with predominant insulin resistance and relative insulin deficiency and type II diabetes mellitus with predominant impaired insulin secretion with or without insulin resistance.
Other specific types of diabetes
Other specific forms of the disease include pathologies with a pronounced genetic component, associated with infectious diseases or taking certain drugs, etc.
Genetic defects in pancreatic β-cell functionthose types of diseases in the development of which a defective gene is clearly established.
Genetic defects in insulin actionthe development of the pathology is related to the peripheral action of insulin, which is impaired due to mutations in the insulin receptor gene.
Diseases of the exocrine pancreas.For example, chronic pancreatitis and other inflammatory pathologies.
Endocrinopathiespathologies associated with excessive secretion of other hormones, such as acromegaly, Cushing's disease, hyperthyroidism.
Diabetes caused by drugs or chemicals, may occur when taking hormonally active substances, α- and β-adrenergic agonists, psychoactive, diuretics and chemotherapeutic drugs.
Diabetes associated with infectious diseases.As a rule, the disease develops due to viral infections (pathogens: Coxsackie, rubella, Epstein Barr viruses).
Unusual forms of immunologically mediated diabetes.For example, immobility and rigidity syndrome, systemic lupus erythematosus.
Other genetic syndromes, sometimes in combination with diabetes.
Gestational diabetes mellitus
It first appears during pregnancy and is characterized by a decrease in the sensitivity of cells to glucose. It is believed that the disease develops due to an imbalance of hormones. After birth, the condition normalizes or may develop into type II diabetes.
Causes of diabetes
Diabetes mellitus develops for a variety of reasons, including genetic and autoimmune diseases, chronic pancreatic disease, and dietary habits.
Common causes of diabetes:
- malfunction of the immune system, which is why it attacks the cells of the pancreas;
- genetic diseases that disrupt the sensitivity of tissues to glucose, change the functioning of the pancreas and reduce or completely stop the synthesis of insulin necessary for the absorption of glucose;
- viral infections Coxsackie viruses, rubella, Epstein Barr, retroviruses can penetrate the cells of the pancreas and destroy the organ;
- chronic diseases that affect the pancreas, cystic fibrosis, pancreatitis, hemochromatosis;
- endocrine diseases Cushing's syndrome, acromegaly;
- toxins (eg rodenticides used to kill rodents, heavy metals, nitrates);
- dietary habits excess of fat and simple carbohydrates in the diet can lead to obesity and decreased sensitivity of cells to insulin;
- drugs, some hormonal drugs (in particular glucocorticosteroids), some drugs for the treatment of diseases of the heart and nervous system, preparations of B vitamins (if consumed in excess).
Risk factors for diabetes
Depending on the type of diabetes, the risk factors for the disease are different.
Risk factors for type I diabetes:
- heredity - the probability of disease is higher if blood relatives have diabetes;
- Some viral infections (eg, rubella, infectious mononucleosis) can trigger an autoimmune reaction in the body, causing the immune system to attack the cells of the pancreas.

Being overweight does not cause type I diabetes, but increases the risk of developing type II diabetes.
The most common risk factors for type II diabetes that are not directly related to an increase in blood sugar levels: overweight, sedentary lifestyle, pregnancy, etc.
During physical activity, glucose is actively broken down to produce energy; substances supplied with food as well as the body's own fat stores are used as a substrate. In obesity, the volume and, accordingly, the area of the membranes of adipose and other cells containing lipid inclusions increases, the relative density of insulin receptors per unit area decreases, as a result of which the cells become less sensitive to insulin and glucose absorption deteriorates.
Risk factors for type II diabetes mellitus:
- overweight and obesity;
- a sedentary lifestyle (without physical activity, glucose is broken down more slowly, so cells can become less sensitive to insulin);
- diabetes mellitus in blood relatives;
- age over 45 years;
- prediabetes is a condition in which the blood glucose level remains at the upper limit of normal for a long time. Prediabetes is considered present if the analysis shows values from 5. 6 to 6. 9 mmol/l;
- diabetes mellitus during pregnancy (gestational diabetes);
- birth of a child weighing more than 4 kg;
- depression;
- cardiovascular diseases;
- arterial hypertension (pressure over 140/90 mm Hg);
- high levels of "bad" high-density cholesterol (more than 0. 9 mmol/l) and triglycerides (more than 2. 82 mmol/l);
- polycystic ovary syndrome.
Symptoms of diabetes
Diabetes mellitus type I usually manifests itself as pronounced symptoms, other types of the disease can develop unnoticed for a long time.
Common symptoms of diabetes:
- strong thirst;
- weakness;
- frequent urination;
- bedwetting in children who have not wet the bed before;
- sudden weight loss for no apparent reason;
- constant strong feeling of hunger;
- frequent urinary tract infections or fungal infections.
Separately, there are the so-called secondary symptoms of diabetes mellitus, which appear in the later stages of the disease and signal complications.
Secondary symptoms of diabetes:
- itchy skin;
- nausea;
- vomiting;
- stomach ache;
- dry mouth;
- muscle weakness;
- blurred vision;
- poorly healing wounds;
- numbness in the fingers or toes;
- acanthosis nigricans darkening of the skin of the neck, armpits, elbows and knees;
- diabetic dermopathy pigment spots with atrophy and peeling of the skin, located on the bends of the lower limbs, often appear due to poor healing of leg wounds;
- Diabetic pemphigus blisters on the lower extremities ranging in size from a few millimeters to a few centimeters. They are most common in elderly patients with long-term diabetes;
- headache;
- smell of acetone from the mouth.

Acanthosis nigricans or darkening of the skin on the neck, knees, elbows and armpits can be a sign of diabetes.
Complications of diabetes
Complications usually develop in patients with advanced diabetes mellitus and include retinopathy, nephropathy, and polyneuropathy.
The destruction of large vessels leads to atherosclerosis, myocardial infarction, stroke and encephalopathy.
Constant monitoring of blood sugar and taking medication to lower its level can prevent or delay the irreversible complications of diabetes.
In addition, the regeneration of small vessels is impaired. Because of this, wounds on the body do not heal well. So even a small cut can turn into a deep festering ulcer.
Diabetic coma
Diabetic coma is a complication of diabetes associated with too high or, conversely, low blood sugar levels.
Depending on the concentration of glucose in the blood, diabetic coma is divided into two types: hypoglycemic (associated with a decrease in sugar levels) and hyperglycemic (caused by an increase in its level).
Hypoglycemic comausually occurs in people with diabetes who are on insulin therapy.
The cause of such a coma is excess insulin, which does not allow the body to raise blood sugar levels to normal levels. This often happens when the dose of insulin is incorrectly calculated or the diet is disturbed, in which the amount of insulin administered does not correspond to the portion of carbohydrates in the food eaten.
Harbingers of hypoglycemic coma:
- body tremors
- chills,
- vertigo,
- nervousness or anxiety
- severe hunger
- nausea
- blurred vision
- heart rhythm disorder.
"Rule 15" for stopping hypoglycemia in diabetes:
If your "sugar" level is reduced, you should eat 15 g of fast carbohydrates (drink juice, take a glucose tablet) and measure your blood sugar after 15 minutes. If it is low, eat another 15 g of fast carbohydrates. Repeat these steps until the sugar rises to at least 3. 9 mmol/l.
In rare cases, low blood sugar can lead to loss of consciousness. In such a situation, he needs an emergency injection of the hormone glucagon, which is carried out by an ambulance.
Some people mistakenly believe that a person in a hypoglycemic coma should pour a sweet liquid into their mouth. However, this is not the case and is fraught with asphyxia (suffocation).
Hyperglycemic comaaccompanied by an acute lack of insulin, which can be caused by severe stress or an insufficient dose of insulin after a meal.

Dangerous hyperglycemia is said to occur if the blood sugar level exceeds 13. 9 mmol/L.
Symptoms of hyperglycemia:
- strong thirst
- frequent urination,
- severe fatigue
- blurred vision
- the smell of acetone or fruity breath,
- nausea and vomiting,
- stomach ache,
- rapid breathing.
If such symptoms appear, you should sit down as soon as possible, ask others to call an ambulance or call an ambulance yourself.
Diagnosis of diabetes mellitus
If a person has symptoms of increased blood sugar concentration: constant thirst, frequent urination, general weakness, blurred vision, numbness of the limbs, you should consult a general practitioner as soon as possible.
But most often diabetes mellitus develops without symptoms, so it is recommended that all people undergo a screening test once a year to detect the disease in the early stages and prevent the development of complications.
Which doctor should I see if I suspect diabetes?
As a rule, people first consult a general practitioner. If diabetes is suspected, he refers them to a specialist who treats metabolic pathologies, an endocrinologist.
During the consultation, the doctor will conduct a study and examination, and to confirm the diagnosis and determine the severity of diabetes, he will prescribe laboratory and instrumental tests.
inspection
If diabetes is suspected, the doctor will clarify the medical history: cases of disease in blood relatives, chronic pathologies of the pancreas, lifestyle, recent infectious diseases.
There are no specific signs of diabetes that can be detected during the examination.
During the examination, the doctor will also assess the condition of the skin: in diabetes mellitus, dark areas of acanthosis nigricans may appear on it. In addition, a specialist can perform a quick glucose test. Exceeding normal values is a reason for a thorough examination.
Laboratory research methods
A blood sugar test is prescribed for diagnosis. Its high level, together with characteristic symptoms such as constant thirst, frequent urination, frequent infectious diseases, is a clear sign of diabetes.
Blood sugar concentration is measured using one of the following tests: fasting and postprandial plasma glucose, glycated hemoglobin level (HbA1c), which reflects the average blood sugar level over the past 3 months.
HbA1c level no more than 6. 0% (42 mmol/l), glucose level no more than 5. 5 mmol/l is considered normal.
In order to make an accurate diagnosis, the examination is carried out at least twice on different days. If the results are ambiguous, a glucose tolerance test is performed, which allows the identification of impaired sensitivity of cells to glucose.
In addition, your doctor may order additional tests to distinguish type 1 diabetes from type 2 diabetes: an autoantibody test and a urine ketone body test.
Antibodies are usually present in people with type I diabetes, and ketone bodies in people with type II diabetes.
To assess the sensitivity of cells to insulin, the doctor can prescribe a test to calculate the HOMA-IR index (Homeostasis model assessment of insulin resistance), which takes into account the level of glucose and insulin in the blood.
If hereditary forms of diabetes are suspected, experts may recommend genetic testing to identify mutations associated with hereditary forms of diabetes mellitus and glucose intolerance.
Instrumental research methods
Instrumental studies help to identify the complications of diabetes: damage to the retina, damage to the heart, blood vessels, kidneys and nerve conduction disorders.
An ultrasound examination of the internal organs is prescribed to assess the condition of the kidneys and pancreas. In addition, the doctor may send the patient for an EKG to detect abnormalities in the heart.
To diagnose visual disturbances, you will need to consult an ophthalmologist. During an ophthalmological examination, the doctor assesses the state of the retina and examines the cornea through a slit lamp or using an ophthalmoscope.
Treatment of diabetes
There is no cure for diabetes. Therapy is aimed at maintaining acceptable blood sugar levels and preventing complications of the disease.
People diagnosed with diabetes must regularly measure their blood sugar levels, inject insulin for type 1 diabetes or take tablets for type 2 diabetes or inject insulin to control their blood sugar levels.
To prevent complications of the disease, the doctor may recommend other drugs. For example, medicines to control blood pressure, thin the blood and prevent cardiovascular disease, as well as medicines that lower blood cholesterol.
Tracking blood sugar levels
Classic glucometers and modern continuous monitoring systems are used to monitor blood sugar levels.
A blood glucose meter is a device equipped with a thin needle. A person pricks his finger with it and drops blood on a special test strip. The glucometer immediately shows the result.
Monitoring systems are sensors that are mounted on the shoulder, stomach or leg. These sensors constantly monitor blood sugar levels. Data from the device is automatically downloaded to a dedicated monitor or phone application. Such devices can signal spikes in blood sugar, draw glucose curves over time, send information to your doctor, and even make recommendations for emergency and routine measures and the need to change diabetes treatment tactics.
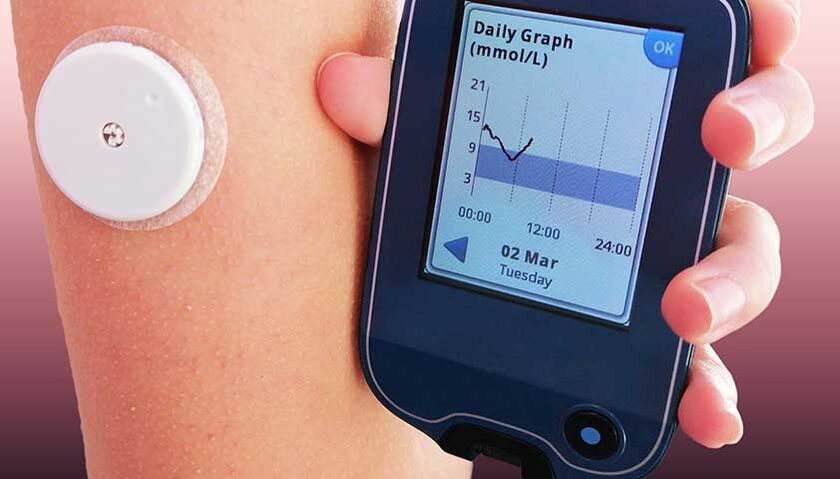
Wearing the monitoring system does not hurt, it is not felt on the body.
Diet for diabetes
There is no special diet for people with diabetes, but it is important for people with this diagnosis to count the amount of carbohydrates they eat each day and keep a food diary.
Counting carbs
Carbohydrates affect blood sugar levels the most, so it is important for people with diabetes not to eliminate them, but to count them.
Carbohydrate counting is the foundation of the diet for people with diabetes who are on insulin therapy. To do this, use the universal parameter unit for bread (XE).
1 XE corresponds to approximately 15 g of net carbohydrates or 20–25 g of bread and raises blood sugar levels by an average of 2. 77 mmol/l. A dose of 1. 4 units of insulin is required for the absorption of such a quantity of glucose.
The amount of carbohydrates in the diet of a person with type I diabetes on average should not exceed 17 bread units per day.
The amount of carbohydrates that a person with diabetes can normally tolerate varies from person to person and depends on weight, level of physical activity, daily caloric needs, and how the body metabolizes carbohydrates.
You can calculate the required amount of carbohydrates per day with a nutritionist or your doctor. After converting the carbohydrates you eat into bread units, your doctor will help you determine the amount of insulin you will need to absorb the glucose. Over time, one will learn to calculate this on their own.
In addition, there are other dietary recommendations for people with diabetes:
- restricting the caloric intake of all overweight patients;
- minimizing the content of fats (mainly of animal origin) and sugars in food;
- consume carbohydrates mainly from vegetables, whole grains and dairy products;
- exclude or limit the consumption of alcoholic beverages (no more than 1 conventional unit for women and 2 conventional units for men per day).
Prediction and prevention of diabetes mellitus
Diabetes mellitus is a chronic disease that cannot be completely cured. But medications and healthier lifestyle changes help avoid complications and slow the progression of the disease.
Without treatment, the prognosis for diabetes mellitus is unfavorable: a person can die due to damage to the cardiovascular system.
Ways to prevent diabetes:
- regular physical activity;
- a varied diet with sufficient fiber, protein, fat and carbohydrates;
- healthy weight control;
- reducing alcohol consumption;
- refusal of alcohol and smoking.
Nutrition for the prevention of type II diabetes
An important part of preventing type II diabetes is a healthy and varied diet. The solid plate principle or method was developed for this purpose.
The healthy plate method divides foods into five main groups: fruits and vegetables, slow-release carbohydrates, dairy products, proteins and fats. You can combine these groups using a regular plate. Fruits and vegetables should make up a third or half of it. Slow carbs a third or a little more. The rest is taken up by dairy products, a little more protein food and a small part of fat.
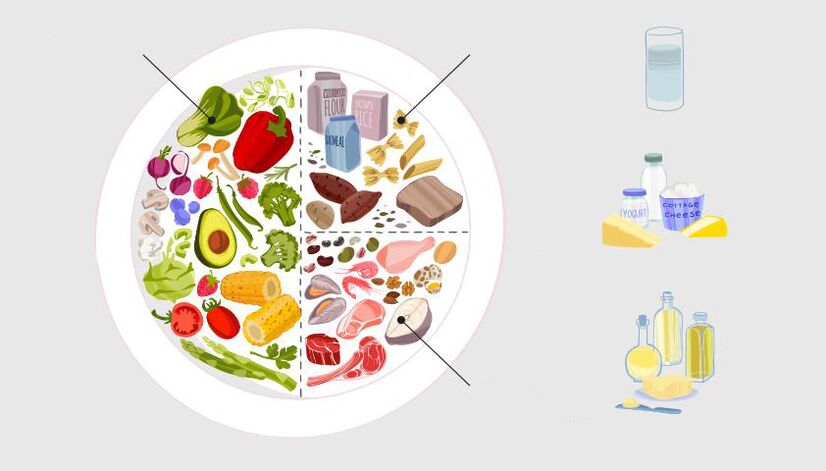
Eating according to the principle of a healthy plate: half is fiber, ⅓ slow carbohydrates, the rest protein foods.
In addition, other important principles of healthy eating must be followed:
- drink according to thirst;
- eat less salt, no more than a teaspoon (5-6 g) per day;
- limit the consumption of trans fats (contained in many ready-made and processed fast foods, cakes and pastries);
- reduce the consumption of saturated fats (contained in sweets, fatty meats, sausages, butter and lard);
- eat less sugar, no more than 7 teaspoons (30 g) a day.
























